 Depo-Provera is the brand name for an injectable contraceptive that contains the hormone progestin. Known as medroxyprogesterone acetate, Depo-Provera prevents ovulation and thickens cervical mucus to prevent sperm from reaching an egg.
Depo-Provera is the brand name for an injectable contraceptive that contains the hormone progestin. Known as medroxyprogesterone acetate, Depo-Provera prevents ovulation and thickens cervical mucus to prevent sperm from reaching an egg.
It’s given as a shot deep into the muscle every three months. It provides highly reliable contraceptive care without needing daily action.
When and Why It’s Used
There are two main reasons Depo-Provera gets prescribed – for birth control and to manage menstrual disorders.
Birth Control
If you wish to prevent pregnancy but don’t want the responsibility of taking a pill every day, Depo-Provera offers set-it-and-forget-it reliability. You simply show up for an injection every three months – no daily alarms to remember contraception.
Among the prime advantages for birth control are:
- No interrupting sex for contraception
- Often lightens periods or stops them altogether
- Potentially Lowers risk of certain cancers
Depo-Provera works incredibly well at preventing pregnancy when you stick to the injection schedule. In a year of typical use, around 6 out of 100 people get pregnant. However, staying on time with follow-up shots is essential for dependability.
Menstrual Disorder Treatment
For issues such as endometriosis, anemia, fibroids, or seizures affected by the menstrual cycle, Depo-Provera helps suppress the endometrium lining growth and prevent ovulation. Benefits include:
- Lowers severity of menstrual cramps and pain
- Lessens heavy menstrual bleeding
- Protects against uterine and endometrial cancers
Your provider may suggest Depo-Provera if other treatments haven’t resolved bothersome period problems.
How It’s Administered
Because Depo-Provera contains only progestin, most women unable to take estrogen oral contraceptives can use it. A prescription and exam from a gynecologist, primary care provider, or women’s health nurse practitioner are necessary to begin.
During the first visit, expect:
- Discussion of complete medical history
- Possible blood pressure check
- Recommendations for the best starting schedule
- Instructions on side effects and follow-up
Guidelines advise getting your first Depo-Provera dose within five days of delivery if postpartum or within five days after your period begins to ensure you aren’t pregnant already. Other start times may require taking a pregnancy test first.
The Injection Procedure
Administering Depo-Provera takes just a minute. Your provider will:
 Clean the injection area with an alcohol pad
Clean the injection area with an alcohol pad- Insert the needle fully into the muscle of your upper arm/hip/buttocks
- Push down the plunger
- Withdraw and apply light pressure
Leave the site alone afterward – no rubbing or massaging.
Follow-Up Plan
During the first week after the initial dose, using a backup contraception method is suggested. This ensures sufficient progestin levels for preventing pregnancy.
Future injections should occur every 12 weeks. Arriving on time is key to dependability. If over 13 weeks pass between shots, it is paramount to take a pregnancy test before the next dose.
What Happens After the Injection
Soon after injection, Depo-Provera enters the bloodstream and starts working using a few mechanisms:
- Blocking LH production to suppress ovulation
- Slowing transport of egg/sperm through fallopian tubes
- Thickening cervical mucus hinders sperm movement
These effects reliably slam the brakes on pregnancy occurrence for three months.
Bleeding Pattern Changes
Many experience lighter, more regular periods or no bleeding at all while on Depo-Provera. But some have prolonged or heavy monthly bleeding for the first 3-6 months before it lessens.
Discuss your bleeding patterns at follow-up visits. Tracking flow on a calendar helps determine if the problems require further assessment by a professional.
Effectiveness and Risk Factors
With on-time injections every three months, fewer than 1 out of 100 Depo-Provera users get pregnant over a year. However, late shots severely undermine dependability.
After week 13, pregnancy risk before the next injection spikes to 6-7%. Going longer with missed doses heightens the odds further. So, sticking tightly to the injection schedule is paramount for efficacy.
Downsides to Consider
While highly effective at preventing pregnancy when appropriately administered, Depo-Provera does come with some disadvantages:
- No protection against sexually transmitted infections
- Delays return to fertility for up to 10 months post-use
- Causes loss of bone mineral density over time, although this is reversible and bone density typically rebounds after discontinuation
Because progestin-only contraceptives seem to lower STD infection barriers in the reproductive tract, barrier methods such as condoms remain necessary to decrease transmission risks if you are worried about contracting an STI.
Additionally, it may take nearly a year after stopping shots before regular ovulation and periods restart due to the long-acting effects of the medroxyprogesterone acetate depot. Those desiring pregnancy soon may wish to consider shorter-acting methods instead.
Common Early Side Effects
During the first 3-6 months, you may experience symptoms such as:
- Breast tenderness
- Headaches
- Mood changes
- Abdominal discomfort
- Irregular spotting
These side effects often progressively resolve as the body adjusts. But notify a provider promptly about serious issues such as breathing difficulties, allergic reactions, blood clots, depression, or heavy bleeding.
Long-term Safety Monitoring
To ensure healthy bone density, gynecologists advise:
 Calcium/vitamin D supplementation
Calcium/vitamin D supplementation- Weight-bearing exercise
- Limiting alcohol/tobacco
These measures counteract bone loss from medroxyprogesterone acetate. Adult women using Depo-Provera for contraception or menstrual problems should plan annual well-woman visits to discuss side effect concerns, bleeding patterns, and the option to switch methods after a few years to avoid bone health impacts.
Consult with Raleigh Gynecology & Wellness to Determine if Depo-Provera Is Right For You
Raleigh Gynecology & Wellness offers personalized guidance in all forms of birth control, from oral contraceptives to long-acting options such as Depo-Provera.
Our top priority is tailoring recommendations to each patient’s unique health status, reproductive goals, and lifestyle.
Contact us today at (919) 636-6670 or set up an appointment online so our team can help you find the reproductive option that best suits your needs.

 If you’re similar to most women, you probably look forward to the onset of your period about as much as a root canal. While menstruation is a normal biological process, that doesn’t make coping with its more unpleasant symptoms, such as migraines, cramps, and heavy bleeding, any easier.
If you’re similar to most women, you probably look forward to the onset of your period about as much as a root canal. While menstruation is a normal biological process, that doesn’t make coping with its more unpleasant symptoms, such as migraines, cramps, and heavy bleeding, any easier. Regulates irregular, unpredictable periods
Regulates irregular, unpredictable periods If frustrating monthly symptoms interfere with feeling your best while hindering your ability to fully participate in academics, careers, relationships, and everything else important to you, don’t hesitate to seek personalized contraceptive guidance.
If frustrating monthly symptoms interfere with feeling your best while hindering your ability to fully participate in academics, careers, relationships, and everything else important to you, don’t hesitate to seek personalized contraceptive guidance. An IUD (intrauterine device) offers safe, effective, l
An IUD (intrauterine device) offers safe, effective, l For your comfort, wear loose-fitting clothing to your insertion appointment. Items such as soft pants, a dress, or a skirt are ideal since they won’t put pressure on your abdomen. You’ll need to remove your clothing below the waist, so wear underwear you don’t mind exposing.
For your comfort, wear loose-fitting clothing to your insertion appointment. Items such as soft pants, a dress, or a skirt are ideal since they won’t put pressure on your abdomen. You’ll need to remove your clothing below the waist, so wear underwear you don’t mind exposing. IUDs free you to enjoy intimacy whenever the mood strikes. Of course, no birth control is 100% perfect at preventing pregnancy.
IUDs free you to enjoy intimacy whenever the mood strikes. Of course, no birth control is 100% perfect at preventing pregnancy. An
An  Once you arrive for your IUD insertion, the real deal begins, but that doesn’t mean you must grit your teeth and bear excruciating pain during the process.
Once you arrive for your IUD insertion, the real deal begins, but that doesn’t mean you must grit your teeth and bear excruciating pain during the process.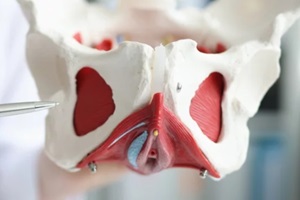 Remember to employ the breathing you practiced to inhale and exhale fully, along with intentionally relaxing your pelvic muscles instead of tensing up.
Remember to employ the breathing you practiced to inhale and exhale fully, along with intentionally relaxing your pelvic muscles instead of tensing up.
 Women who might want to have more kids can select a shorter-acting IUD of 3-5 years.
Women who might want to have more kids can select a shorter-acting IUD of 3-5 years. When it comes to family planning, being informed, empowered, and in control of your fertility is invaluable. IUDs offer women in Raleigh a convenient and personalized way to shape their families on their terms.
When it comes to family planning, being informed, empowered, and in control of your fertility is invaluable. IUDs offer women in Raleigh a convenient and personalized way to shape their families on their terms.