Essential Takeaways:
- Research confirms that underwire bras are not linked to breast cancer or other serious breast conditions.
- The comfort and fit of your bra have a greater effect on your well-being than whether it contains an underwire.
- Normal bra wear, including underwire styles, does not block lymphatic drainage or trap toxins in breast tissue.
- Factors like genetics, aging, and pregnancy influence breast shape more than the type of bra you wear.
- Consistent screenings, self-checks, and wearing supportive, comfortable bras are the best ways to care for your breast health.
 You probably wear a bra most days without thinking twice. However, stories in the media that claim that underwires could be “bad for your breasts” may raise concerns. Maybe you’ve heard that they block lymph flow, cause chronic pain, or even increase the risk of breast cancer. It’s understandable to wonder if there’s any truth behind these rumors. When it comes to your breast health, it’s natural to want to take all precautions.
You probably wear a bra most days without thinking twice. However, stories in the media that claim that underwires could be “bad for your breasts” may raise concerns. Maybe you’ve heard that they block lymph flow, cause chronic pain, or even increase the risk of breast cancer. It’s understandable to wonder if there’s any truth behind these rumors. When it comes to your breast health, it’s natural to want to take all precautions.
So, do underwire bras really affect your breast health? Find out what the research actually says and what matters most for your comfort and long-term well-being.
The Myth: Underwire Bras and Breast Cancer
One of the most common concerns about underwire bras is the effect of the wire against the torso. The wire has been thought to compress lymph nodes, trapping “toxins” and raising the risk of breast cancer. However, there is little scientific evidence to support these claims.
A landmark study from the Fred Hutchinson Cancer Research Center found no link between bra-wearing habits, including the use of underwire bras, and breast cancer risk in postmenopausal women. Researchers examined factors such as hours of daily wear, age at first bra use, and bra type and found no association.
Similarly, Harvard Health Publishing reviewed the data. It concluded that no link was seen between the risk of either invasive ductal carcinoma or lobular carcinoma with regard to bra wearing, including use of an underwire.
The Real Issue: Comfort, Fit, and Support
Even though underwires are not believed to be dangerous, that doesn’t mean every bra is good for you. The real impact of a bra on your body has more to do with fit than with design.
If your bra leaves red marks, digs into your skin, or feels uncomfortable by midday, that’s a sign that something is off. Poorly fitted bras can cause shoulder and neck pain, possible posture issues, and chronic skin irritation. These issues do not just affect women who wear underwire bras but can be worse if the wire presses too tightly against the ribs or breast tissue.
In fact, many women regularly wear the wrong bra size and don’t know it. According to the Chiropractic & Osteopathy journal, around 80% of women are wearing bras that don’t fit correctly. A properly fitted bra should support you without pinching, digging, or slipping.
If you’ve had breast surgery, radiation, or lymph node removal, your healthcare provider might recommend avoiding underwire bras for a while to allow healing. That’s less about the wire itself and more about preventing friction on sensitive tissue.
What About Lymph Flow and Sagging?
You may have heard claims that wearing underwire bras, or any bras, can block lymphatic drainage or make breasts sag faster. Current research does not support these ideas either.
Lymphatic drainage happens through deep channels in the body, not the surface areas where a bra sits. There’s no evidence that typical bra pressure, even from underwires, restricts that flow in healthy women.
As for sagging, it’s influenced by genetics, age, pregnancy, breastfeeding, and gravity, not by whether you wear a bra. A French study from the University of Besancon even suggested that consistent bra use doesn’t prevent sagging and might slightly affect natural ligament tone, although more research is needed.
What You Can Do for Better Breast Health
You don’t need to toss all your underwire bras. Instead, focus on these healthy habits that truly support your breast well-being:
-
 Get fitted regularly. Your body changes over time due to weight shifts, hormones, and aging, all of which can affect breast size and shape. A professional fitting every year or two helps keep your bras supportive and comfortable.
Get fitted regularly. Your body changes over time due to weight shifts, hormones, and aging, all of which can affect breast size and shape. A professional fitting every year or two helps keep your bras supportive and comfortable. - Listen to your body. If your bra feels too tight, causes soreness, or leaves indentations, it’s time to adjust your size or try a different style.
- Take breaks when you want to. There’s no medical need to wear a bra all day, every day. If you’re at home and comfortable without one, that’s perfectly fine.
- Keep up with screenings. Mammograms, self-awareness, and regular checkups do far more for early detection than any bra choice ever could.
- Choose what makes you feel confident. Whether that’s an underwire bra, a soft bralette, or going wire-free entirely, your comfort and confidence are part of good breast health.
Received Specialized Care at Raleigh Gynecology & Wellness
There’s no credible scientific evidence that underwire bras harm your breast health or increase cancer risk. What matters most is wearing bras that fit well, support you comfortably, and make you feel good in your own body.
If you’re experiencing discomfort, noticing changes, or just want professional guidance on maintaining breast health, our women’s health specialists are here for you. Schedule a visit today to review your breast health and get personalized comfort recommendations.


 Hormonal changes and a slower metabolism can result in weight gain, most commonly in the abdominal area, raising the risk of type 2 diabetes and insulin resistance. Balanced nutrition, portion awareness, and regular movement help reduce that risk.
Hormonal changes and a slower metabolism can result in weight gain, most commonly in the abdominal area, raising the risk of type 2 diabetes and insulin resistance. Balanced nutrition, portion awareness, and regular movement help reduce that risk. Menopause marks a new chapter, not the end of health and vitality. By staying proactive with screenings, lifestyle habits, and supportive care, you can protect your well-being for years.
Menopause marks a new chapter, not the end of health and vitality. By staying proactive with screenings, lifestyle habits, and supportive care, you can protect your well-being for years. For many women, the thought of menopause can bring feelings of uncertainty or even worry. It’s a natural transition that every woman experiences, yet the
For many women, the thought of menopause can bring feelings of uncertainty or even worry. It’s a natural transition that every woman experiences, yet the  During menopause, the ovaries stop releasing eggs and produce less estrogen, which can lead to both emotional and physical changes. Common symptoms include hot flashes, brain fog, changes in hair or skin, weight fluctuations, and a decrease in libido. Some women notice shifts in mood or energy levels, while others may experience few symptoms at all.
During menopause, the ovaries stop releasing eggs and produce less estrogen, which can lead to both emotional and physical changes. Common symptoms include hot flashes, brain fog, changes in hair or skin, weight fluctuations, and a decrease in libido. Some women notice shifts in mood or energy levels, while others may experience few symptoms at all. Menopause is a transitional stage in every woman’s life, and with the proper care, it can be managed confidently and comfortably. Embracing each stage and learning how your body responds can help you maintain balance and overall well-being.
Menopause is a transitional stage in every woman’s life, and with the proper care, it can be managed confidently and comfortably. Embracing each stage and learning how your body responds can help you maintain balance and overall well-being. When you come in for breast cancer screening, your
When you come in for breast cancer screening, your 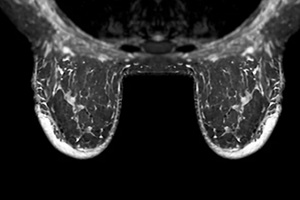 These are reassuring classifications. BI-RADS 1 means no suspicious findings; BI-RADS 2 means there is a benign (noncancerous) feature such as a stable cyst or benign calcification.
These are reassuring classifications. BI-RADS 1 means no suspicious findings; BI-RADS 2 means there is a benign (noncancerous) feature such as a stable cyst or benign calcification. Stay on schedule. If the report calls for follow-up imaging (for BI-RADS 0 or 3), showing up for these
Stay on schedule. If the report calls for follow-up imaging (for BI-RADS 0 or 3), showing up for these 
 While many women find relief through lifestyle changes, there are times when symptoms become severe or significantly impact daily life, such as intense mood swings, persistent sleep problems, or unbearable hot flashes. If this sounds familiar, consider seeking professional support.
While many women find relief through lifestyle changes, there are times when symptoms become severe or significantly impact daily life, such as intense mood swings, persistent sleep problems, or unbearable hot flashes. If this sounds familiar, consider seeking professional support.